Meeting the needs of complex peripheral artery disease: The devices and decisions needed for optimizing outcomes
Approaching complex PAD
Discussing patient considerations, best practices, and device placement techniques.
Arun Chervu, MD, MBA, MHA, FACS
What types of cases do you see in your practice on any given day?
We see a combination of both claudication and critical limb ischemia (CLI) requiring urgent intervention. For claudicants, my first approach is to try conservative medical therapy including smoking cessation, medications, and an exercise program. Although it’s not a structured exercise program, I give them an idea of what they need to do and try medications, including cilostazol. For some patients, I’m able to put off intervention for 6 months to a year, sometimes 2 years, and then do the appropriate intervention at that time.
We do a lot of peripheral artery disease (PAD) work, but there are always surprises, and it’s really important to be ready for them. Then, we hopefully can treat the patient in one sitting rather than bringing him or her back at a separate time. That’s why having a full armamentarium—covered stents, self-expanding stents, balloon-expandable stents—is an important part of taking care of the patient with PAD and complex PAD, which we’re seeing more of.
What are some of the disease characteristics and comorbidities that move a PAD case from being simple to complex?
We have real difficulty with patients with end-stage renal disease; those are a very challenging group of patients. Diabetes is pretty standard in our patients, and congestive heart failure, stroke, and coronary artery disease are significant comorbidities.
It can be difficult to treat some of these patients, especially those with CLI and multilevel disease. Sometimes they require hybrid intervention—a combination with an iliac stent and a bypass. In an outpatient setting, it’s sometimes hard to know what you’re going to do. We can fix certain aspects of the disease, but then we need to move the case over to a hybrid OR setting.
What are the first signs of multilevel disease you see in a patient?
A lot of it starts with the history—how long they’ve had issues with claudication, how long they’ve had issues with development of an ulcer. Then, the imaging is where you have an initial sense. We typically don’t do CT scans, but if you do an aortic ultrasound or an arterial study, you start getting an idea of multilevel disease. You also can tell when you watch the patient walk.
What are some of the considerations when you have a patient with long-segment superficial femoral artery (SFA) disease?
One of the considerations always is whether to cover the collaterals. I don't think that debate is ever going to be completely settled one way or the other—you can make arguments for each side. One argument to cover them is that you are then providing a great bypass, so that you really never get rid of them. The other argument is that if you can save them, why not?
When it comes to complex, occlusive disease, what is your game plan?
Everyone handles chronic total occlusions differently. I prefer a simple MEDLINE KUMPE® Access Catheter or BOSTON SCIENTIFIC RUBICON® Support Catheter, and then I go through with the TERUMO® GLIDEWIRE® Hydrophilic Coated Guidewire and do balloon angioplasty. This works over 90% of the time. I have used a reentry catheter on occasion.
When do you make the choice to use a covered stent graft or a bare-metal stent?
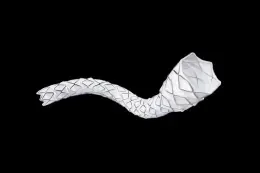
In the SFA and popliteal space, the decision is not always easy because there are multiple characteristics to consider. The standard go-to is a self-expanding stent. You start thinking about using a covered stent for long lesions and in-stent restenosis (ISR) and a GORE® VIABAHN® Endoprosthesis in particular if you have a long occlusion (10–15 cm or longer). The VIASTAR randomized study demonstrated the advantages of the GORE VIABAHN Endoprosthesis compared to bare-metal stents in long lesions.1 A lot of data have shown those patients do better at 1 year, 2 years, 3 years, and so on with a GORE VIABAHN Endoprosthesis. The concern with patients with very significant plaque is whether you can dilate that area with a balloon or if atherectomy is needed to get rid of the lesion.
I also like using a GORE VIABAHN Endoprosthesis in the case of ISR. By physically preventing cells from infiltrating the lumen of the device, it addresses the underlying cause of the ISR. Plus, because it's ISR, the chance to "leave nothing behind" is not available. This approach is supported by data from the RELINE study (which remains one of the only randomized studies for any device in ISR), which demonstrated that the GORE VIABAHN Endoprosthesis is capable of durably treating ISR.2 At 2 years, the primary patency was 60% for the GORE VIABAHN Endoprosthesis compared to only 10% for PTA. In my mind, this is where the GORE VIABAHN Endoprosthesis separates itself from paclitaxel therapies, which, as the DEBATE-ISR study showed, do not carry the 12-month benefits out to years 2 and 3.3
When do you choose a GORE VIABAHN Endoprosthesis to reline a failed bare-metal stent? Do you do anything else besides using a covered stent graft?
There are times when I will just do plain balloon angioplasty, especially if it’s a short lesion (< 5 or 6 cm in length). If I've done balloon angioplasty once already and the restenosis returns, then I'm more likely to put in a covered stent.
Some physicians do atherectomy on ISR lesions, but I don't particularly love that concept. I don't want it to get stuck in the struts, especially proximally/distally.
The problem with ISR is intimal hyperplasia. A very short-segment ISR can be treated with balloon angioplasty. Some people use laser atherectomy debulking, but I think a lot of those patients come back very early, and that's where a covered stent has an advantage.
The advantage of a GORE VIABAHN Endoprosthesis for a long lesion is that you are covering the area of the disease in the intimal hyperplasia, and that really is better in the long run and hopefully will stimulate less reaction to the ongoing tissue in that area—the vascular endothelial cells.
What do you consider when you're trying to optimize stent placement?
Covering all diseased portions of the SFA is important when using the GORE VIABAHN Endoprosthesis. Leaving a diseased proximal SFA will more likely lead to early stent thrombosis. Optimizing stent placement to the origin of the SFA can be done using magnified and oblique views to more accurately see the profunda and SFA origins. Intravascular ultrasound is a very helpful tool in selected cases. We have gotten better at sizing the stent grafts, which was a problem in the initial adaptation with GORE VIABAHN Endoprosthesis. Intravascular ultrasound or quantitative angiography has helped us get a better idea of sizing so that we are not oversizing > 20%.
It is important to know the length of the lesion to ensure you are intraluminal distally and sizing properly. Making sure you have good inflow and outflow is really important. We cover everything we balloon, and that's another important aspect—try not to balloon outside the device.
You have to be careful that you don't go between the stent and the arterial wall. These challenges can occur when you try to cross lesions, especially stent separation or stent fracture. It's very important to stay intraluminal.
There are a number of technical mishaps or hurdles that you need to avoid when stent fractures or a separation occur. You want to stay in the middle of the stent. You don't want to go through the stent interstices. It’s helpful to get magnified views. Get multiple rotation views so you know that you're inside, and then try to put a catheter through. The catheter typically will not go if you are in the stent interstices, so that's really important because it’s hard to crush the stent regardless of what you use, unless it's a small stent in a big artery.
What is your algorithm for follow-up and long-term surveillance, especially for covered stents?
I think the same algorithm applies for almost all stents. If I'm worried about something, I'll do an arterial study at 1 month, an ankle-brachial index, and an arterial duplex. If things seem reasonable, then I'll go out to 3 months, 6 months, 9 months, 1 year, and then every 6 months after that for at least another 1 or 2 years. It all depends on what you find. If there is severe recurrent stenosis, then we would want to reintervene to save the intervention we've done. We are looking at primary intervention, secondary intervention, primary patency, and secondary patency.
What outcomes or lifestyle changes do your patients experience after revascularization?
Patients come in with myriad symptoms prior to any intervention, and not all of it is straightforward claudication. Some people say their legs or buttocks ache. Some people say they are fatigued. Not everybody gives a classic history of, “My calf hurts when I walk half a block.”
There are a couple of things that people report after revascularization. Some patients report that they have pain where they have had balloon angioplasty. They have pain in the calf or thigh. However, I would say in the majority of patients, those symptoms are gone, and they report that they’re walking better within about a week. That's what we want to see—less pain when they walk in the calves and the thigh, depending on what you revascularize. Most patients are happy with the outcomes, and they tend to stay happy as long as there is no compromise of the arterial circulation. Quality of life is the reason we perform many of the cases.
- Lammer J, Zeller T, Hausegger KA, et al. Heparin-bonded covered stents versus bare-metal stents for complex femoropopliteal artery lesions: the randomized VIASTAR trial (Viabahn endoprosthesis with PROPATEN bioactive surface [VIA] versus bare nitinol stent in the treatment of long lesions in superficial femoral artery occlusive disease). J Am Coll Cardiol. 2013;62:1320-1327.
- Bosiers M, Deloose K. 2-year results of the RELINE trial comparing Viabahn stent-grafts to POBA for ISR show durable benefits to endograft treatment. Presented at: 41st Annual VEITHsymposium; November 18-22, 2014; New York, NY.
- Grotti S, Liistro F, Angioli P, et al. Paclitaxel-eluting balloon vs standard angioplasty to reduce restenosis in diabetic patients with in-stent restenosis of the superficial femoral and proximal popliteal arteries: three-year results of the DEBATE-ISR study. Journal of Endovascular Therapy 2016;23(1):52-57.
Products listed may not be available in all markets.
See all products by region:

Arun Chervu, MD, MBA, MHA, FACS
Director, Clinical Trials
Vascular Surgical Associates
Marietta, Georgia
Disclosures: On the clinical trials and speakers bureau for Gore & Associates.