MR Conditional
GORE® VIABAHN® Endoprosthesis with PROPATEN Bioactive Surface* Case Studies
Image
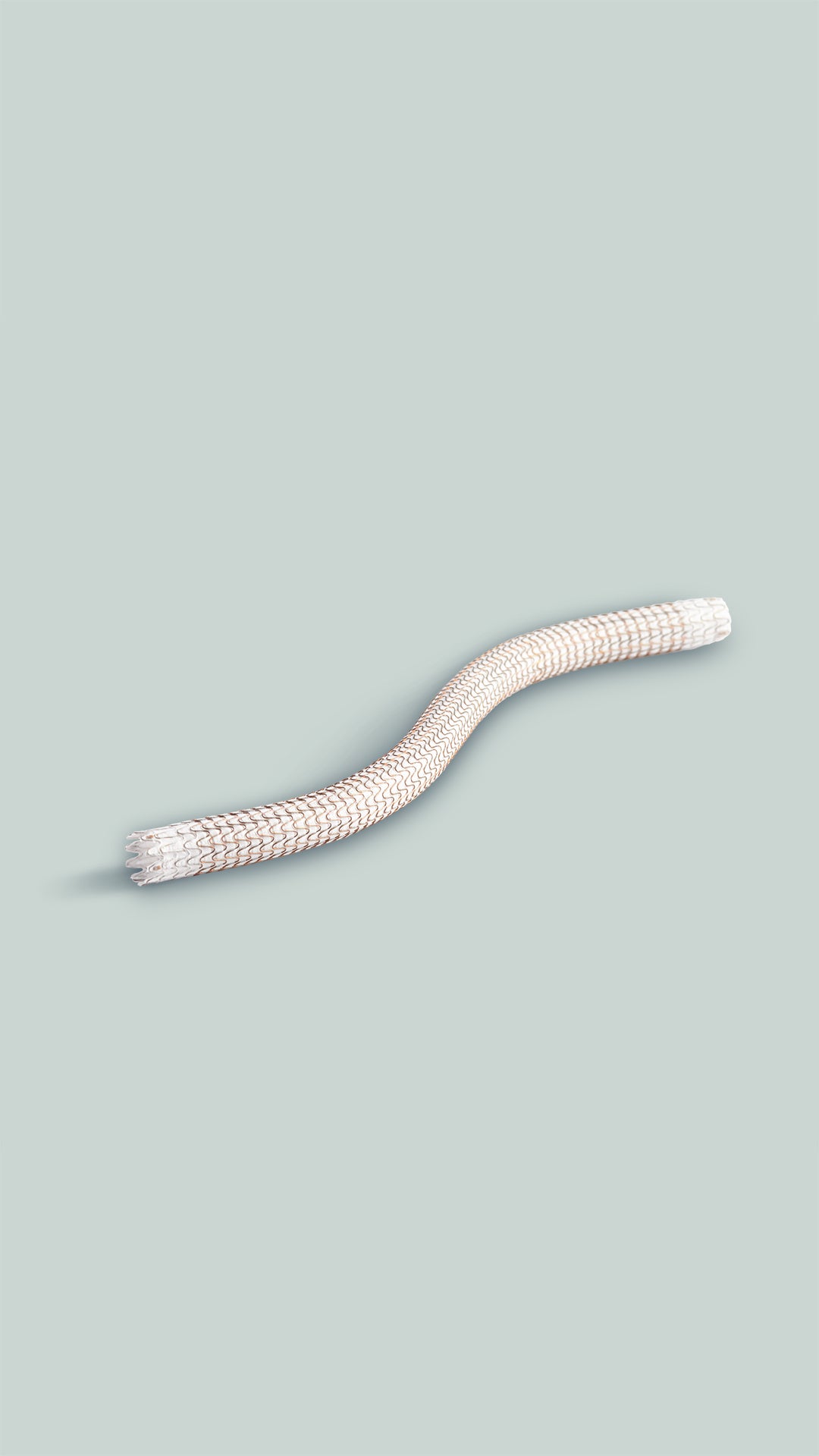
The VIABAHN® Device enables you to deliver high patency and durable outcomes to minimize reinterventions for your patients.
The cases presented feature a range of challenges that demonstrate the proven performance of the VIABAHN® Device.
AV graft lesions across the elbow
PTA failures of AV graft lesions
Thrombosed AV grafts
Chronic total SFA occlusions
Long SFA lesions
In-stent restenosis of the SFA
*As used by Gore, PROPATEN Bioactive Surface refers to Gore's proprietary CBAS® Heparin Surface.
Refer to Instructions for Use at eifu.goremedical.com for a complete description of all applicable indications, warnings, precautions and contraindications for the market where this product is available. RXOnly
INDICATIONS FOR USE IN EUROPE:
The GORE® VIABAHN® Endoprosthesis with PROPATEN Bioactive Surface is indicated for the treatment of:
- de novo or restenotic lesions in the iliac arteries
- de novo or restenotic lesions in the superficial femoral artery and proximal popliteal artery
- in-stent restenotic lesions in the superficial femoral artery and proximal popliteal artery
- stenosis or thrombotic occlusion at the venous anastomosis of synthetic arteriovenous (AV) access grafts and in the venous outflow of dialysis access circuits, including the central veins
- popliteal artery aneurysms and isolated visceral artery aneurysms
- traumatic or iatrogenic vessel injuries in arteries that are located in the chest cavity, abdominal cavity, or pelvis (except for aorta, coronary, innominate, carotid, vertebral, and pulmonary arteries)
CONTRAINDICATIONS:
- Non-compliant lesions where full expansion of an angioplasty balloon catheter was not achieved during pre-dilatation, or where lesions cannot be dilated sufficiently to allow passage of the delivery system.
- Do not use the GORE® VIABAHN® Endoprosthesis with PROPATEN Bioactive Surface in patients with known hypersensitivity to heparin, including those patients who have had a previous incident of Heparin-Induced Thrombocytopenia (HIT) type II.
Product may not be available in all countries. Please check with your Gore representative for availability