GORE® VIABAHN®Endoprosthesis with PROPATEN Bioactive Surface* Clinical Data
Open more possibilities with the VIABAHN® Device
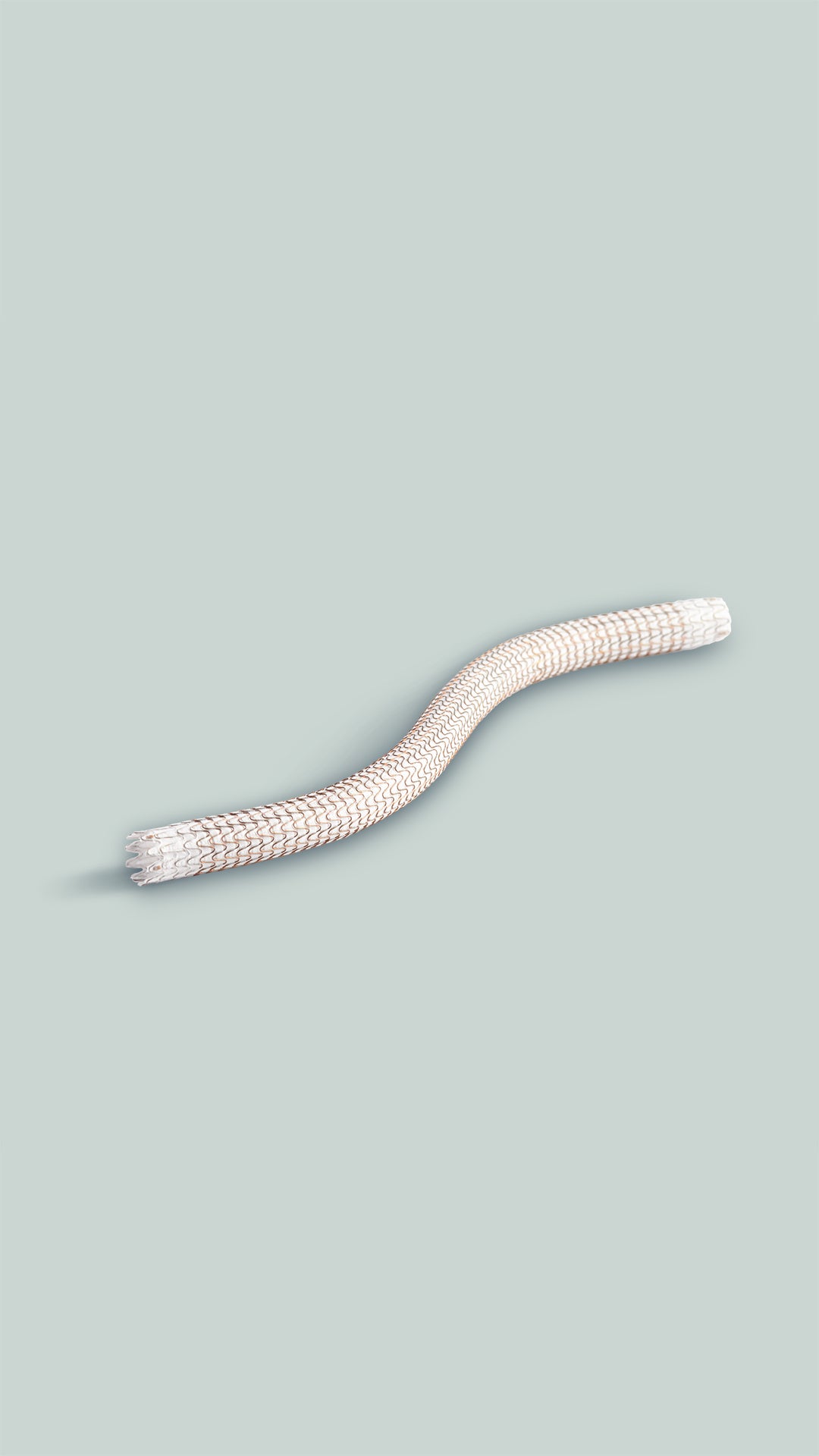
Proven across a broad range of complex cases, the versatility of the VIABAHN® Device enables you to deliver high patency and durable outcomes to minimize reinterventions.
Consider the types of cases you treat and the challenges they present; the VIABAHN® Device helps you optimize clinical outcomes for your patients.
Arteriovenous (AV) access
The VIABAHN® Device has proven success in the most challenging AV access cases, including early percutaneous transluminal angioplasty (PTA) failures, lesions at points of flexion and in thrombosed grafts.
Designed to conform to challenging anatomy and proven to resist fractures†
Demonstrated patency independent of the number of prior interventions1
Increased primary patency in thrombosed grafts of both the target lesion and the circuit when compared to PTA1
Superficial femoral artery (SFA)
The VIABAHN® Device delivers strong clinical performance in the most challenging cases with 80% average primary patency§ demonstrated across seven multicenter, prospective, randomized or single-arm studies with an average lesion length of 23 cmI and 71% chronic total occlusions (CTOs).2-8
Comparable clinical results to above knee surgical bypass (both prosthetic and native vein)2,9
Excellent patency and durability independent of lesion length2-6
In-stent restenosis (ISR) of the SFA
The VIABAHN® Device provides durable treatment for complex in-stent restenotic lesions.10,11
Ability to cover and seal disease, leading to durable outcomes in long, complex ISR10,11
Iliac artery
The VIABAHN® Device is indicated to treat stenotic iliac lesions.
The VIABAHN® Device family has demonstrated patency that approaches surgical bypass outcomes.12-14
Publications
Your resource for current publications and clinical data demonstrating the utility of the VIABAHN® Device in practice.
Twelve-month outcomes from the Japanese post-market surveillance study of the Viabahn Endoprosthesis as treatment for symptomatic peripheral arterial disease in the superficial femoral arteries
Iida O, Ohki T, Soga Y, et al. Twelve-month outcomes from the Japanese post-market surveillance study of the Viabahn Endoprosthesis as treatment for symptomatic peripheral arterial disease in the superficial femoral arteries. Journal of Endovascular Therapy 2022;29(6):855-865.
Long-term results of the Japanese multicenter Viabahn trial of heparin bonded endovascular stent grafts for long and complex lesions in the superficial femoral artery
Ohki T, Kichikawa K, Yokoi H, et al. Long-term results of the Japanese multicenter Viabahn trial of heparin bonded endovascular stent grafts for long and complex lesions in the superficial femoral artery. Journal of Vascular Surgery 2021;74(6):1958-1967.e2.
Stent-grafts are the best way to treat complex in-stent restenosis lesions in the superficial femoral artery: 24-month results from a multicenter randomized trial
Bosiers M, Deloose K, Callaert J, et al. Stent-grafts are the best way to treat complex in-stent restenosis lesions in the superficial femoral artery: 24-month results from a multicenter randomized trial. Journal of Cardiovascular Surgery 2020;61(5):617-625.
Clinical and economic benefits of stent grafts in dysfunctional and thrombosed hemodialysis access graft circuits in the revise randomized trial
Mohr BA, Sheen AL, Roy-Chaudhury P, Schultz SR, Aruny JE; REVISE Investigators. Clinical and economic benefits of stent grafts in dysfunctional and thrombosed hemodialysis access graft circuits in the REVISE Randomized Trial. Journal of Vascular & Interventional Radiology 2018;30(2):203-211.e4.
Outcomes of the Japanese multicenter Viabahn trial of endovascular stent grafting for superficial femoral artery lesions
Ohki T, Kichikawa K, Yokoi H, et al. Outcomes of the Japanese multicenter Viabahn trial of endovascular stent grafting for superficial femoral artery lesions. Journal of Vascular Surgery 2017;66(1):130-142.e1.
1-year results of a multicenter randomized controlled trial comparing the heparin-bonded endoluminal bypass to the femoropopliteal bypass
Reijnen MMPJ, van Walraven LA, Fritschy WM, et al. 1-year results of a multicenter randomized controlled trial comparing heparin-bonded endoluminal to femoropopliteal bypass. JACC: Cardiovascular Interventions 2017;10(22):2320-2331.
Sustained benefit at 2 years for covered stents versus bare-metal stents in long SFA lesions: the VIASTAR trial
Lammer J, Zeller T, Hausegger KA, et al. Sustained benefit at 2 years for covered stents versus bare-metal stents in long SFA lesions: the VIASTAR trial. Cardiovascular & Interventional Radiology 2015;38(1):25-32.
Heparin-bonded, expanded polytetrafluoroethylene-lined stent graft in the treatment of femoropopliteal artery disease: 1-year results of the VIPER (Viabahn Endoprosthesis with Heparin Bioactive Surface in the treatment of Superficial Femoral Artery Obstructive Disease) Trial
Saxon RR, Chervu A, Jones PA, et al. Heparin-bonded, expanded polytetrafluoroethylene-lined stent graft in the treatment of femoropopliteal artery disease: 1-year results of the VIPER (Viabahn Endoprosthesis with Heparin Bioactive Surface in the Treatment of Superficial Femoral Artery Obstructive Disease) Trial. Journal of Vascular & Interventional Radiology 2013;24(2):165 173.
* As used by Gore, PROPATEN Bioactive Surface refers to Gore’s proprietary CBAS® Heparin Surface.
† Across all uses, the GORE® VIABAHN® Endoprosthesis has a reported fracture rate of 0.0013% (data on file 2025; W. L. Gore & Associates, Inc; Flagstaff, AZ.)
‡ One-year weighted average primary patency.
I Weighted average lesion length.
- Vesely T, DaVanzo W, Behrend T, Dwyer A, Aruny J. Balloon angioplasty versus Viabahn stent graft for treatment of failing or thrombosed prosthetic hemodialysis grafts. Journal of Vascular Surgery 2016;64(5):1400-1410.e1. http://www.sciencedirect.com/science/article/pii/S0741521416301756
- Reijnen M, van Walraven L, Fritschy W, et al. 1-year results of a multicenter, randomized controlled trial comparing heparin-bonded endoluminal to femoropopliteal bypass. Journal of Cardiovascular Interventions 2107;10(22):2320-2331.
- Ohki T, Kichikawa K, Yokoi H, et al. Long-term results of the Japanese multicenter Viabahn trial of heparin bonded endovascular stent grafts for long and complex lesions in the superficial femoral artery. Journal of Vascular Surgery 2021;74(6):1958-1967.e2.
- Saxon RR, Chervu A, Jones PA, et al. Heparin-bonded, expanded polytetrafluoroethylene-lined stent graft in the treatment of femoropopliteal artery disease: 1-year results of the VIPER (Viabahn Endoprosthesis with Heparin-bonded Bioactive Surface in the Treatment of Superficial Femoral Artery Obstructive Disease) Trial. Journal of Vascular & Interventional Radiology 2013;24(2):165-173.
- Lammer J, Zeller T, Hausegger KA, et al. Sustained benefit at 2 years for covered stents versus bare-metal stents in long SFA lesions: the VIASTAR Trial. Cardiovascular & Interventional Radiology 2015;38(1):25-32.
- Zeller T, Peeters P, Bosiers M, et al. Heparin-bonded stent-graft for the treatment of TASC II C and D femoropopliteal lesions: the Viabahn-25 cm Trial. Journal of Endovascular Therapy 2014;21(6):765-774.
- Iida O, Ohki T, Soga Y, et al. Twelve-month outcomes from the Japanese post-market surveillance study of the Viabahn Endoprosthesis as treatment for symptomatic peripheral arterial disease in the superficial femoral arteries. Journal of Endovascular Therapy 2022;29(6):855-865.
- Iida O, Takahara M, Soga Y, et al; VANQUISH Investigators. One-year outcomes of heparin-bonded stent-graft therapy for real-world femoropopliteal lesions and the association of patency with the prothrombotic state based on the prospective, observational, multicenter Viabahn Stent-Graft Placement for Femoropopliteal Diseases Requiring Endovascular Therapy (VANQUISH) Study. Journal of Endovascular Therapy 2021;28(1):123-131.
- McQuade K, Gable D, Pearl G, Theune B, Black S. Four-year randomized prospective comparison of percutaneous ePTFE/nitinol self-expanding stent graft versus prosthetic femoral-popliteal bypass in the treatment of superficial femoral artery occlusive disease. Journal of Vascular Surgery 2010;52(3):584-591.
- Bosiers M, Deloose K, Callaert J, et al. Stent-grafts are the best way to treat complex in-stent restenosis lesions in the superficial femoral artery: 24-month results from a multicenter randomized trial. The Journal of Cardiovascular Surgery 2020;61(5):617-25
- Soukas P, Becker M, Stark K, Tepe G; RELINE MAX Investigators. Three-year results of the GORE® VIABAHN® endoprosthesis in the superficial femoral artery for in-stent restenosis. Journal of the Society for Cardiovascular Angiography & Interventions 2023;2(6)Part A:101183.
- Lammer J, Dake M.D., Bleyn J, et al. Peripheral arterial obstruction: prospective study of treatment with a transluminally placed self-expanding stent graft. Radiology 2000;217(1):95-104.
- Bismuth J, Gray BH, Holden A, Metzger C, Panneton J; VBX FLEX Study Investigators. Pivotal study of a next-generation balloon-expandable stent-graft for treatment of iliac occlusive disease. Journal of Endovascular Therapy 2017;24(5):629-637. Pivotal Study of a Next-Generation Balloon-Expandable Stent-Graft for Treatment of Iliac Occlusive Disease - Jean Bismuth, Bruce H. Gray, Andrew Holden, Christopher Metzger, Jean Panneton, , on behalf of the VBX FLEX Study Investigators, on behalf of the VBX FLEX Study Investigators, 2017
- Indes JE, Pfaff MJ, Farrokhyar F, et al. Clinical outcomes of 5358 patients undergoing direct open bypass or endovascular treatment for aortoiliac occlusive disease: a systematic review and meta-analysis. Journal of Endovascular Therapy 2013;20(4):443-455.
Golchehr B, Zeebregts CJ, Reijnen MMPJ, Tielliu IFJ. Long-term outcome of endovascular popliteal artery aneurysm repair. Journal of Vascular Surgery 2018;67(6):1797-1804.
Refer to Instructions for Use at eifu.goremedical.com for a complete description of all applicable indications, warnings, precautions and contraindications for the markets where this product is available. RXOnly
INDICATIONS FOR USE IN EUROPE: The GORE® VIABAHN® Endoprosthesis with PROPATEN Bioactive Surface is indicated for the treatment of:
- de novo or restenotic lesions in the iliac arteries
- de novo or restenotic lesions in the superficial femoral artery and proximal popliteal artery
- in-stent restenotic lesions in the superficial femoral artery and proximal popliteal artery
- stenosis or thrombotic occlusion at the venous anastomosis of synthetic arteriovenous (AV) access grafts and in the venous outflow of dialysis access circuits, including the central veins
- popliteal artery aneurysms and isolated visceral artery aneurysms
- traumatic or iatrogenic vessel injuries in arteries that are located in the chest cavity, abdominal cavity, or pelvis (except for aorta, coronary, innominate, carotid, vertebral, and pulmonary arteries)
CONTRAINDICATIONS:
- Non-compliant lesions where full expansion of an angioplasty balloon catheter was not achieved during pre-dilatation, or where lesions cannot be dilated sufficiently to allow passage of the delivery system.
- Do not use the GORE® VIABAHN® Endoprosthesis with PROPATEN Bioactive Surface in patients with known hypersensitivity to heparin, including those patients who have had a previous incident of Heparin-Induced Thrombocytopenia (HIT) type II.