Product Value Summary
GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface*
Clinical and economic value in dialysis access
For end-stage renal disease (ESRD) patients who require regular hemodialysis, maintaining a functioning dialysis access circuit is essential.
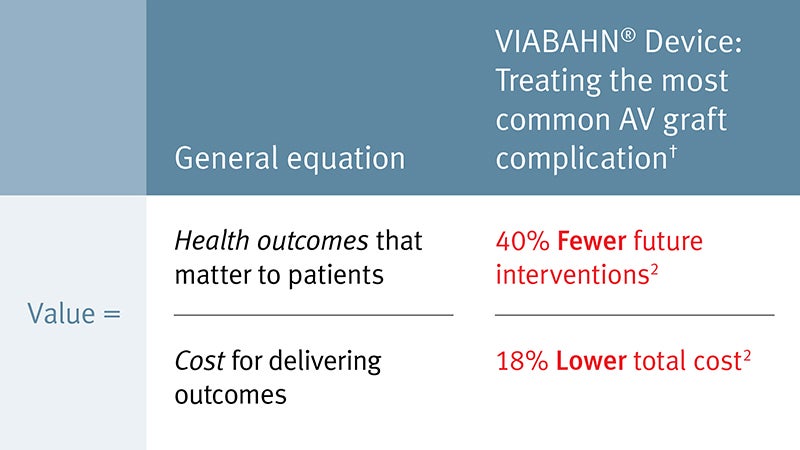
In patients who use arteriovenous (AV) grafts for hemodialysis, the VIABAHN® Device can increase clinical value by improving patency1 and reducing the number of future interventions when compared to percutaneous transluminal angioplasty (PTA).2
When treating one of the most common complication of AV grafts,† the VIABAHN® Device demonstrated 40% fewer future interventions2 which resulted in an 18% reduction of total costs over two years compared to PTA ($30,329 versus $37,206; P = .027).2
18% reduction of total costs versus PTA over two years:
$30,329 versus $37,206 per patient (P = .027)2
The Future of Value Analysis
A Handbook for Health Care Professionals
Read perspectives from value analysis professionals who share their thoughts regarding the importance of effective collaboration, paradigm shifts with determining value, and the critical focus on the future of healthcare.

* As used by Gore, Heparin Bioactive Surface refers to Gore’s proprietary CBAS Heparin Surface.
† AV graft thrombosis occurs when blood stops flowing through the AV graft, resulting in an inability to perform hemodialysis treatment. In the Gore REVISE Clinical Study, graft thrombosis was the most common indication for patient enrollment.1
- Vesely T, DaVanzo W, Behrend T, Dwyer A, Aruny J. Balloon angioplasty versus Viabahn stent graft for treatment of failing or thrombosed prosthetic hemodialysis grafts. Journal of Vascular Surgery 2016; 64(5):1400-1410.e1. http://www.sciencedirect.com/science/article/pii/S0741521416301756
- Mohr BA, Sheen AL, Roy-Chaudhury P, Schultz SR, Aruny JE; REVISE Investigators. Clinical and economic benefits of stent grafts in dysfunctional and thrombosed hemodialysis access graft circuits in the REVISE Randomized Trial. Journal of Vascular & Interventional Radiology 2019;30(2):203-211.e4. https://www.jvir.org/article/S1051-0443(18)31772-X/fulltext
Refer to Instructions for Use at eifu.goremedical.com for a complete description of all applicable indications, warnings, precautions and contraindications for the markets where this product is available. RXOnly
INDICATIONS FOR USE IN THE U.S.: The GORE® VIABAHN® Endoprosthesis and the GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface are indicated for improving blood flow in patients with symptomatic peripheral arterial disease in superficial femoral artery de novo and restenotic lesions up to 270 mm in length with reference vessel diameters ranging from 4.0 - 7.5 mm. The GORE® VIABAHN® Endoprosthesis and the GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface are indicated for improving blood flow in patients with symptomatic peripheral arterial disease in superficial femoral artery in-stent restenotic lesions up to 270 mm in length with reference vessel diameters ranging from 4.0 - 6.5 mm. The GORE® VIABAHN® Endoprosthesis and the GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface are indicated for improving blood flow in patients with symptomatic peripheral arterial disease in iliac artery lesions up to 80 mm in length with reference vessel diameters ranging from 4.0 - 12 mm. The GORE® VIABAHN® Endoprosthesis and the GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface are also indicated for the treatment of stenosis or thrombotic occlusion at the venous anastomosis of synthetic arteriovenous (AV) access grafts.
CONTRAINDICATIONS: The GORE® VIABAHN® Endoprosthesis and the GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface are contraindicated for non-compliant lesions where full expansion of an angioplasty balloon catheter was not achieved during pre-dilatation, or where lesions cannot be dilated sufficiently to allow passage of the delivery system. Do not use the GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface in patients with known hypersensitivity to heparin, including those patients who have had a previous incident of Heparin-Induced Thrombocytopenia (HIT) type II.
