AV Access
Achieve rapid arteriovenous (AV) access and limit catheter use
Gore Dialysis AV Access Solutions offer support for individualized care
With Gore Dialysis Access Solutions, you can achieve reliable arteriovenous access (AV access) quickly while adhering to the National Kidney Foundation’s updated Kidney Disease Outcomes Quality Initiative (KDOQI) clinical practice guidelines, which recommend an individualized approach to patient care.1
The updated KDOQI guidelines recommend a patient-first approach and support AV grafts (AVG) as a practical, frontline solution for complex cases, including patients with challenging revisions, chronic comorbidities or limited vein options.1
Gore Dialysis AV Access Solutions include:

Should a fistula always be first?
As end-stage renal disease (ESRD) becomes more prevalent, and patient populations become more complex, both using a central venous catheter (CVC) and achieving successful arteriovenous fistula (AVF) maturation have become increasingly challenging.
CHALLENGES WITH CVC
68% of patients
still on CVC after 3 months2
CHALLENGES WITH AVF
50% of AVFs
require intervention to mature3
48% of patients
initiating with CVC have more access procedures4
Shorter
secondary patency following intervention compared to AVGs3
4.5x more
hospitalizations for catheter-related bacteremia4
More interventions
per year compared to AVGs3
Compared with AVGs
CVCs are associated with a 49% higher risk of fatal infections due to complications5
When do KDOQI guidelines recommend going straight-to-graft?
Updated KDOQI guidelines recommend patient-first, individualized care that helps to preserve vessels for future access creation and avoid unnecessary procedures and complications. When risk factors indicate that a patient may not experience the intended benefits of an AVF due to likely maturation challenges, vascular grafts can offer an access solution that works for your patient.
Complex dialysis cases
Gore supports evolved dialysis access protocols with dialysis access solutions that help you achieve rapid access, immediate cannulation and reliable repair with dependable outcomes.
78%
One study reported, using the GORE® PROPATEN® Vascular Graft, 78% patency at 1 year6
54%
The GORE® ACUSEAL Vascular Graft demonstrated 54% fewer CVC dependent days versus standard grafts7,8
50%
Greater than 50% reduction in catheter time with early cannulation grafts, compared with standard grafts9
46%
Higher secondary patency and a 46% reduction in catheter days with AVGs maturing without intervention, compared with AVFs requiring intervention to mature3
Expand your dialysis access options
- Lok CE, Huber TS, Lee T, et al. KDOQI Vascular Access Guideline Work Group. KDOQI Clinical Practice Guideline for Vascular Access: 2019 update. American Journal of Kidney Diseases 2020;75(4)Supplement 2:S1-S164.
- United States Renal Data System (USRDS) website. 2020 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2020. Accessed November 30, 2020. https://adr.usrds.org/2020
- Harms J, Rangarajan S, Young CJ, Barker-Finkel J, Allon M. Outcomes of arteriovenous fistulas and grafts with or without intervention before successful use. Journal of Vascular Surgery 2016;64(1):155-162.
- Mohr BA, Sheen AL, Roy-Chaudhury P, Schultz SR, Aruny JE. REVISE Investigators. Clinical and economic benefits of stent grafts in dysfunctional and thrombosed hemodialysis access graft circuits in the REVISE Randomized Trial. Journal of Vascular & Interventional Radiology 2019;30(2):203-211.e4.
- Ravani P, Palmer SC, Oliver MJ, et al. Associations between hemodialysis access type and clinical outcomes: a systematic review. Journal of the American Society of Nephrology 2013;24(3):465-473.
- Davidson I, Hackerman C, Kapadia A, Minhajuddib A. Heparin bonded hemodialysis e-PTFE grafts result in 20% clot free survival benefit. The Journal of Vascular Access 2009;10(3):153-156.
- Quinn B, Cull DL, Carsten CG. Hemodialysis access: placement and management complications. In: Hallet JW Jr, Mills JL, Earnshaw J, Reekers JA, Rooke T, eds. Comprehensive Vascular & Endovascular Surgery. 2nd ed. Philadelphia, PA: Mosby; 2009;(26):429-462.
- Shingarev R, Mayal D, Barker-Finkel J, Allon M. Arteriovenous graft placement in predialysis patients: a potential catheter-sparing strategy. American Journal of Kidney Diseases 2011;58(2):243-247.
- Mohapratra A, You TH, Lowenkamp MN, et al. Cost-effectiveness analysis of immediate access arteriovenous grafts versus standard grafts for hemodialysis. Journal of Vascular Surgery 2021;73(2):581-587.
- Glickman MH, Burgess J, Cull D, Roy-Chaudhury P, Schanzer H. Prospective multicenter study with a 1-year analysis of a new vascular graft used for early cannulation in patients undergoing hemodialysis. Journal of Vascular Surgery 2015;62(2):434-441.
- Tozzi M, Franchin M, Ietto G, et al. Initial experience with the Gore® Acuseal graft for prosthetic vascular access. Journal of Vascular Access 2015;16(6):467-471.
- Maytham GGD, Sran HK, Chemla ES. The use of the early cannulation prosthetic graft (AcusealTM) for angioaccess for haemodialysis. Journal of Vascular Access 2015;62(2):434-441.
- Vesely T, DaVanzo W, Behrend T, Dwyer A, Aruny J. Balloon angioplasty versus Viabahn stent graft for treatment of falling or thrombosed prosthetic hemodialysis grafts. Journal of Vascular Surgery 2013;64(5):1400-1410.e1. https://wwww.sciencedirect.com/science/arcle/pii/S074152141630156. Accessed August 23, 2021.
Refer to Instructions for Use at eifu.goremedical.com for a complete description of all applicable indications, warnings, precautions and contraindications for the markets where this product is available. RXOnly
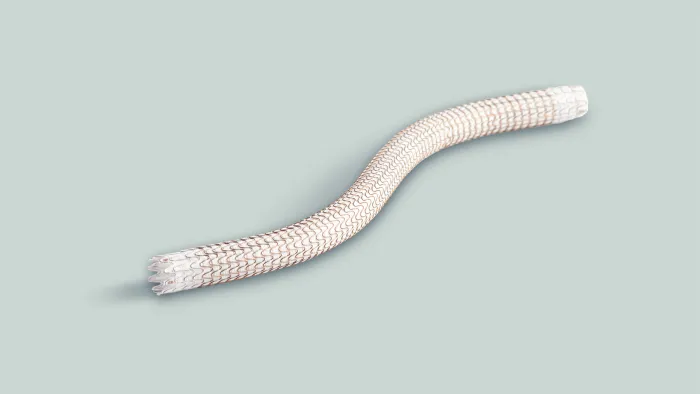
GORE® ACUSEAL Vascular Graft
INDICATIONS FOR USE IN THE U.S.: GORE® ACUSEAL Vascular Graft is intended for use as a vascular prosthesis in patients requiring vascular access.
CONTRAINDICATIONS:DO NOT use the GORE® ACUSEAL Vascular Graft in patients with known hypersensitivity to heparin, including those patients who have had a previous incident of Heparin-Induced Thrombocytopenia (HIT) type II. DO NOT use GORE® ACUSEAL Vascular Graft as a patch. If cut and used as a patch, GORE® ACUSEAL Vascular Grafts may lack adequate transverse strength.
GORE® PROPATEN® Vascular Graft
INDICATIONS FOR USE IN THE U.S.: GORE® PROPATEN® Vascular Grafts are intended for use as vascular prostheses for replacement or bypass of diseased vessels in patients suffering occlusive or aneurysmal diseases, in trauma patients requiring vascular replacement, for dialysis access, or for other vascular procedures.
CONTRAINDICATIONS: DO NOT use the GORE® PROPATEN® Vascular Graft in patients with known hypersensitivity to heparin, including those patients who have had a previous incidence of Heparin-Induced Thrombocytopenia (HIT) type II. DO NOT use any configuration of GORE® PROPATEN® Vascular Grafts with Removable Rings, Non-Removable Rings or Integrated Rings for coronary artery bypass or cerebral reconstruction procedures. DO NOT use GORE® PROPATEN® Vascular Grafts as a patch. If cut and used as a patch, GORE® PROPATEN® Vascular Grafts may lack adequate transverse strength.
FOR PATCHING APPLICATIONS: For cardiovascular procedures requiring patch materials, use the appropriate GORE® ACUSEAL Cardiovascular Patch.
GORE® VIABAHN® Endoprosthesis
INDICATIONS FOR USE IN THE U.S.: The GORE® VIABAHN® Endoprosthesis is indicated for improving blood flow in patients with symptomatic peripheral arterial disease in superficial femoral artery de novo and restenotic lesions up to 270 mm in length with reference vessel diameters ranging from 4.0 – 7.5 mm, in superficial femoral artery in-stent restenotic lesions up to 270 mm in length with reference vessel diameters ranging from 4.0 – 6.5 mm, and in iliac artery lesions up to 80 mm in length with reference vessel diameters ranging from 4.0 – 12 mm. The GORE® VIABAHN® Endoprosthesis is also indicated for the treatment of stenosis or thrombotic occlusion at the venous anastomosis of synthetic arteriovenous (AV) access grafts.
CONTRAINDICATIONS: The GORE® VIABAHN® Endoprosthesis is contraindicated for noncompliant lesions where full expansion of an angioplasty balloon catheter was not achieved during pre-dilatation, or where lesions cannot be dilated sufficiently to allow passage of the delivery system. Do not use the GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface in patients with known hypersensitivity to heparin, including those patients who have had a previous incidence of Heparin-Induced Thrombocytopenia (HIT) type II.